Guided Tissue Bone Regeneration (GTBR) is a procedure using membranes and grafts to restore lost bone and tissue, aiding dental implants and treating periodontal disease, promoting natural healing.
1.1 Definition and Overview of GTBR
Guided Tissue Bone Regeneration (GTBR) is a surgical procedure designed to restore lost bone and tissue, particularly in cases of periodontal disease or trauma. It involves the use of barrier membranes to guide the healing process, ensuring that bone and tissue regenerate effectively. This technique leverages biological and mechanical principles to create an environment conducive to natural repair. GTBR is widely used in dental implantology and periodontal treatment, offering a minimally invasive approach to reconstruct damaged areas. By promoting regeneration, it enhances stability for dental implants and improves overall oral health, making it a cornerstone in modern reconstructive dentistry.
1.2 Historical Development and Evolution
Guided Tissue Bone Regeneration (GTBR) has evolved significantly since its inception in the mid-20th century. Early concepts emerged in the 1950s and 1960s, with pioneers like Hurley and Melcher exploring bone regeneration principles. The 1980s marked a breakthrough with the introduction of barrier membranes, distinguishing GTBR from traditional grafting methods. Since then, advancements in biomaterials, resorbable membranes, and growth factors have refined the technique. Modern GTBR integrates biologic agents and tissue engineering, offering enhanced predictability and minimally invasive approaches. This evolution reflects a growing understanding of bone biology and regeneration, making GTBR a cornerstone in contemporary dental and medical reconstruction.
Principles of Guided Tissue Bone Regeneration
Guided Tissue Bone Regeneration relies on biological and mechanical principles to facilitate bone and tissue growth, utilizing barriers and biologics to optimize healing and regeneration processes effectively.
2.1 Biological Principles
Guided Tissue Bone Regeneration is rooted in biological principles that promote tissue repair and regeneration. It involves the use of stem cells, growth factors, and osteogenic cells to stimulate bone formation. The process utilizes natural healing mechanisms, such as osteoinduction, osteoconduction, and osteogenesis, to create a conducive environment for tissue growth. Membranes and grafts act as barriers and scaffolds, guiding cells to regenerate lost bone and tissue. This approach ensures that cells migrate and differentiate effectively, leading to the restoration of functional bone and tissue structures. Biological factors like BMPs (Bone Morphogenetic Proteins) play a crucial role in enhancing regeneration outcomes.
2.2 Mechanical Principles
The mechanical principles of GTBR focus on stabilizing the graft material and ensuring proper tissue integration. This involves the use of barriers and scaffolds to isolate the regeneration area, preventing unwanted cell migration. Mechanical stability is crucial for bone healing, as movement can disrupt the regeneration process. The structural framework provided by membranes and grafts helps maintain space for tissue growth. Additionally, mechanical principles ensure that the graft remains securely in place, promoting optimal bone formation. These principles work in tandem with biological factors to create a stable environment for tissue regeneration, enhancing the overall success of the procedure.
Applications of GTBR in Dental and Medical Fields
GTBR is widely used in dental implantology, treating periodontal disease, and repairing bone defects. It also supports jaw reconstruction, enhancing stability for implants and restoring tissue health effectively.
3.1 Dental Implantology
Guided Tissue Bone Regeneration (GTBR) plays a crucial role in dental implantology by enabling the reconstruction of deficient alveolar bone, ensuring sufficient support for dental implants. This technique is particularly beneficial for patients with insufficient bone density due to periodontal disease or trauma. By using barrier membranes and bone grafts, GTBR guides the growth of new bone tissue, creating a stable foundation for implants; This approach minimizes the need for larger bone grafts and simplifies the surgical process, leading to faster recovery times and more predictable outcomes for patients seeking implant-based tooth replacement solutions.
3.2 Treatment of Periodontal Disease
Guided Tissue Bone Regeneration (GTBR) is a cornerstone in the treatment of periodontal disease, addressing bone loss and tissue destruction caused by infection. By using barrier membranes and bone grafts, GTBR promotes the regeneration of lost bone and periodontal ligaments, stabilizing teeth and preventing further progression of the disease. This technique is particularly effective for patients with advanced periodontal defects, offering a minimally invasive solution to restore oral health. GTBR not only halts disease progression but also enhances aesthetic and functional outcomes, enabling patients to retain their natural teeth and regain a healthy, stable smile.

Materials and Techniques Used in GTBR
GTBR employs biocompatible membranes, bone grafts, and growth factors to promote bone and tissue regeneration, ensuring proper healing and structural support for dental implants or damaged areas.
4.1 Membranes and Barrier Materials
Membranes and barrier materials are essential in GTBR, preventing soft tissue invasion into defect sites. They are designed to promote bone regeneration by creating a protected environment. Biocompatible materials like collagen or synthetic polymers are commonly used, ensuring tissue compatibility and durability. These membranes can be resorbable or non-resorbable, with resorbable options eliminating the need for removal. They often incorporate growth factors to enhance healing. The membrane’s structure and properties are critical for guiding tissue growth and stabilizing the graft material, ensuring optimal bone regeneration and structural restoration in dental and periodontal applications.
4.2 Bone Grafting Materials
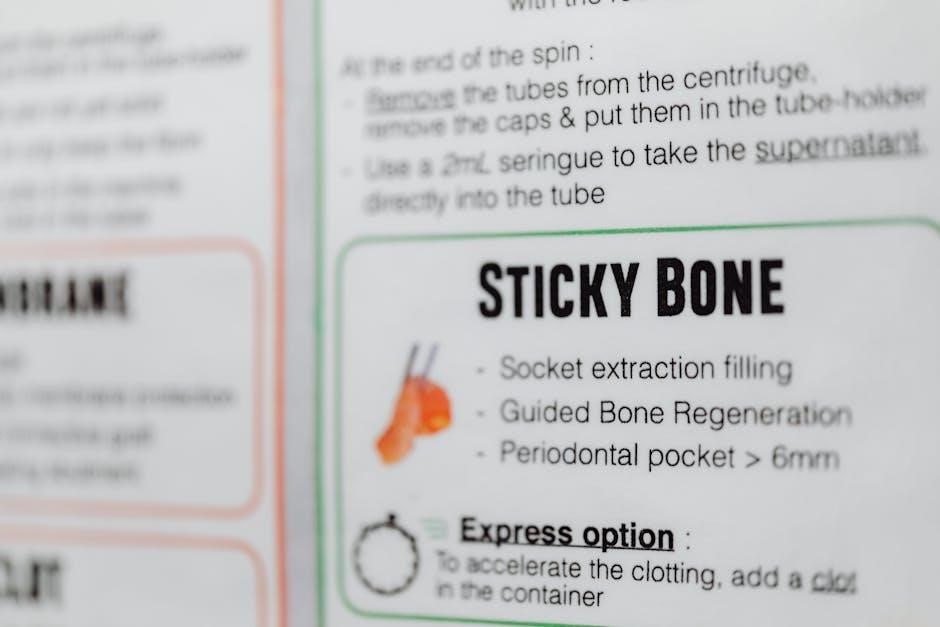
Bone grafting materials are crucial in GTBR for filling bone defects and promoting regeneration. Common materials include autografts (patient’s own bone), allografts (donor bone), xenografts (animal-derived), and alloplasts (synthetic); Each material has unique properties and applications. Autografts are gold standard for osteogenic potential, while allografts and xenografts offer accessibility and reduced morbidity. Alloplasts, like hydroxyapatite and titanium, provide durability and compatibility. These materials act as scaffolds, supporting cell migration and bone formation. Advances in biomaterials have enhanced their integration and bioactivity, improving bone regeneration outcomes in dental and periodontal procedures. They are often combined with membranes to optimize defect filling and tissue repair.
4.3 Growth Factors and Biologic Agents
Growth factors and biologic agents play a pivotal role in GTBR by enhancing bone healing and tissue regeneration. Platelet-derived growth factor (PDGF) and bone morphogenetic proteins (BMPs) are commonly used to stimulate cellular activity. These agents promote osteogenesis by recruiting stem cells and increasing collagen synthesis. Biologic agents are often combined with bone grafts to improve integration and regeneration rates; Their ability to accelerate healing makes them invaluable in complex dental procedures, such as implant placements and periodontal treatments. Advances in biologic therapies continue to refine GTBR outcomes, offering tailored solutions for patients with diverse bone deficiency challenges.

Surgical Procedure and Techniques
Guided Tissue Bone Regeneration involves precise surgical techniques, such as incision, membrane placement, and bone grafting, to regenerate bone and tissue, enhancing implant stability and aesthetic outcomes effectively.
5.1 Pre-Surgical Planning and Preparation
Pre-surgical planning for GTBR involves detailed imaging, such as CBCT scans, to assess bone density and defect morphology. Patient evaluation includes medical history, smoking habits, and overall health. Treatment goals are defined, and surgical approaches are customized. Anesthesia options and surgical tools are prepared. Post-operative care instructions are provided, emphasizing dietary restrictions and oral hygiene. This phase ensures optimal conditions for the procedure, minimizing risks and enhancing outcomes. Proper preparation is critical for the success of the regeneration process and patient recovery.
5;2 Surgical Implementation
The surgical procedure begins with an incision to access the bone defect. A resorbable or non-resorbable membrane is carefully placed over the defective area to guide tissue regeneration. Bone grafting materials are then filled into the defect to promote new bone formation. The membrane is secured, ensuring proper tension and coverage. Advanced techniques, such as pin fixation, may be used for stability. The incision is closed with sutures, and the site is protected to prevent infection. Precision and care are critical during implementation to ensure optimal regeneration and integration of the grafts with the surrounding tissue.
5.3 Post-Surgical Care and Recovery
Post-surgical care is crucial for optimal healing in GTBR. Patients are advised to rest, avoid strenuous activities, and adhere to a soft-food diet for several weeks. The surgical site should be protected from trauma or dislodgement. Gentle oral hygiene practices are encouraged, avoiding direct contact with the treated area. Follow-up appointments are scheduled to monitor healing progress and remove any sutures or membranes. Recovery typically lasts 3-6 months, depending on the extent of the procedure. Proper adherence to post-surgical instructions ensures successful bone and tissue regeneration, minimizing complications and promoting a stable foundation for dental implants or natural teeth.
Advantages and Benefits of GTBR
Guided Tissue Bone Regeneration offers enhanced bone and tissue repair, improving dental implant stability and providing a minimally invasive solution for patients with bone loss.
6.1 Improved Bone and Tissue Regeneration
Guided Tissue Bone Regeneration enhances bone healing by using membranes and grafts to promote natural tissue repair. This technique fosters bone density and structure restoration, enabling better support for dental implants. It also aids in repairing damaged gum and soft tissue, preventing further deterioration. The use of growth factors and stem cells further accelerates healing, ensuring a more predictable and successful outcome. By focusing on regenerative principles, GTBR provides a biologically friendly environment for tissue and bone to thrive, leading to improved oral health and functional stability.
6.2 Enhanced Stability for Dental Implants
Guided Tissue Bone Regeneration significantly enhances the stability of dental implants by restoring lost bone and tissue. This procedure ensures a solid foundation for implants, improving osseointegration and long-term durability. By addressing bone deficiencies, GTBR allows for optimal implant placement, even in cases of severe bone loss. The regenerated bone provides enhanced structural support, reducing the risk of implant failure. This approach is particularly beneficial for patients with insufficient bone structure, offering a reliable solution for achieving stable and functional dental restoration. The use of membranes and grafts ensures a predictable outcome, making GTBR a cornerstone in modern implantology.
6.3 Minimally Invasive Approach
Guided Tissue Bone Regeneration offers a minimally invasive approach to restore lost bone and tissue, reducing surgical trauma and promoting faster recovery. Advanced techniques and materials, such as membranes and biocompatible grafts, enable precise tissue guidance with smaller incisions. This method minimizes damage to surrounding tissues, leading to less post-operative discomfort and shorter healing times. The use of growth factors and biologic agents further enhances the body’s natural healing process. By optimizing surgical precision, GTBR provides a patient-friendly solution, making it an attractive option for individuals seeking effective bone and tissue regeneration with minimal invasion and reduced recovery time.

Challenges and Limitations
GTBR faces challenges like patient-specific factors, biological limitations, and mechanical complexities, requiring precise technique and material selection to ensure successful bone and tissue regeneration outcomes.
7.1 Biological and Mechanical Challenges
Biological challenges in GTBR include insufficient bone density and compromised healing capacity due to factors like age or disease. Mechanical challenges involve membrane stability and graft integration difficulties. Ensuring proper membrane placement and material compatibility is crucial for successful regeneration. Additionally, the risk of membrane exposure or graft failure can impede healing. Addressing these challenges requires careful patient selection, advanced surgical techniques, and the use of high-quality biomaterials. Researchers continuously explore innovative solutions to overcome these limitations and enhance GTBR outcomes.
7.2 Patient-Specific Factors
Patient-specific factors significantly influence GTBR outcomes, including age, overall health, and systemic conditions like diabetes. Smoking and poor oral hygiene can impede healing. Anatomical limitations, such as insufficient bone density or jaw structure, also pose challenges. Additionally, compliance with post-surgical care and the patient’s ability to avoid harmful habits play a critical role. These factors must be carefully evaluated during pre-surgical planning to ensure personalized treatment and optimal results. Addressing these individual challenges is essential for achieving successful bone and tissue regeneration.
Future Directions and Innovations
Future advancements in GTBR include biomaterials, stem cell therapy, and tissue engineering. These innovations aim to enhance bone and tissue regeneration, improving outcomes and minimizing invasiveness.
8.1 Advances in Biomaterials
Recent advancements in biomaterials for GTBR focus on developing biocompatible and bioactive materials that promote tissue integration and bone growth. Researchers are exploring materials like nanomodified bone grafts and bioresorbable membranes that dissolve over time, reducing the need for secondary surgeries. Additionally, biomaterials that release growth factors gradually are being developed to enhance regeneration efficiency. These innovations aim to improve the predictability and success rates of GTBR procedures, offering more sustainable and effective solutions for bone reconstruction.
8.2 Stem Cell Therapy and Tissue Engineering
Stem cell therapy and tissue engineering are emerging as groundbreaking approaches in GTBR, offering novel solutions for bone and tissue regeneration. Stem cells, capable of differentiating into bone and periodontal cells, are being explored for their potential to enhance healing. Tissue engineering involves designing bioactive scaffolds that guide cellular growth and tissue formation; These advancements aim to create tailored treatments that regenerate bone and tissue more effectively, potentially reducing recovery time and improving surgical outcomes. Innovations in this field are paving the way for more personalized and biologically driven solutions in GTBR.
Guided Tissue Bone Regeneration (GTBR) has revolutionized the approach to bone and tissue reconstruction, offering precise and effective solutions for dental and medical applications. By leveraging biological and mechanical principles, GTBR enhances natural healing processes, ensuring improved outcomes for patients with bone loss or periodontal disease. The integration of advanced materials, such as membranes and bone grafts, along with emerging innovations like stem cell therapy, underscores the potential for further advancements. As research continues, GTBR remains a cornerstone in modern regenerative medicine, providing hope for patients seeking durable and aesthetically pleasing results.
